Antibiotic Susceptibility Profile of Carbapenem-Resistant Klebsiella pneumoniae Isolates after Exposure to Non-Thermal Plasma
DOI:
https://doi.org/10.23851/mjs.v36i1.1583Keywords:
Nonthermal plasma, Carbapenem resistance, Klebsiella pneumoniae, Antibiotic, Bacteria, AntibacterialAbstract
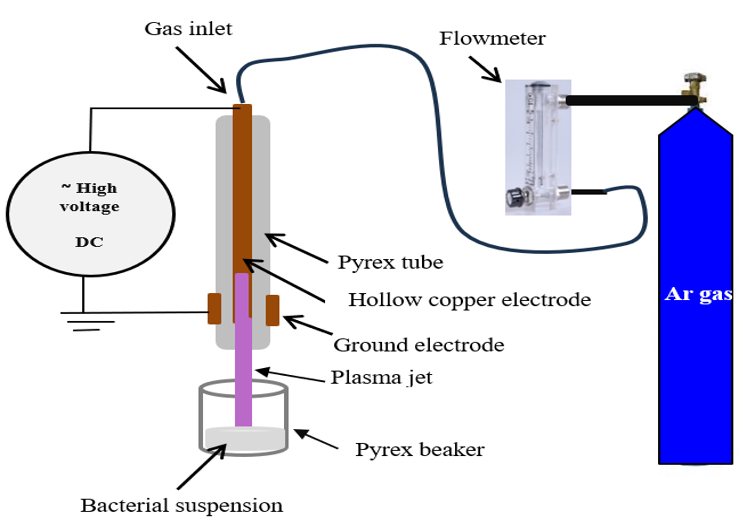
Background: Carbapenem-resistant Klebsiella pneumoniae (CRKP) should be considered an emerging clinical threat. Because these isolates are resistant to nearly all commonly used antibiotics, control of their spread is important. Objective: This study aimed to examine the impact of non-thermal plasma on the CRKP isolates from Iraqi patients. Methods: A total of 150 specimens were collected from different clinical sources. Thirty isolates of K. pneumoniae were obtained in this study. The antibiotic susceptibility testing was conducted using Kirby-Bauer’s disk diffusion method before exposing the isolates to non-thermal plasma for 15, 30, 60, 90, and 120 seconds at a temperature of 37 °C for 24 hours. Results: The results of the study suggested that K. pneumoniae isolates exhibited differential antibiotic susceptibility following treatment with a nonthermal plasma. Both piperacillin, ceftazidime, and imipenem demonstrated increased efficacy 15 seconds after exposure with an inhibition rate of 100%, while ciprofloxacin and gentamicin showed optimal efficacy with inhibition rates of 97% and 90%, respectively. However, amikacin displayed resistant phenotypes at 15 seconds with an inhibition rate of 87%, and the inhibition rate with tetracycline and cefepime was the same at 83%; as for the time of 30 seconds and above, all nine tested antibiotics showed an inhibition rate of 100%. Conclusions: The results demonstrate the important impact of nonthermal plasma on the antibiotic susceptibility profiles of K. pneumoniae isolates. Understanding the role of nonthermal plasma in antibiotic resistance can help in developing more effective strategies for controlling infections caused by multi-resistant organisms. Further research is needed to clarify the underlying processes and their implications for treatment.
Downloads
References
M. Romance, M. U. Khan, M. S. Islam, M. F. Islam, and M. H. Haque, "Draft genome sequence of multidrug-resistant Klebsiella pneumoniae Hakim-RU strain isolated from a patient with urinary tract infections in Bangladesh," Microbiology Resource Announcements, vol. 13, no. 5, p. e0008924, 2024.
CrossRef | PubMed
S. Yoo, K.-M. Lee, N. Kim, T. N. Vu, R. Abadie, and D. Yong, "Designing phage cocktails to combat the emergence of bacteriophage-resistant mutants in multidrug-resistant Klebsiella pneumoniae," Microbiology Spectrum, vol. 12, no. 1, p. e0125823, 2024.
CrossRef | PubMed
T. Sawa, K. Kooguchi, and K. Moriyama, "Molecular diversity of extended-spectrum β-lactamases and carbapenemases, and antimicrobial resistance," Journal of Intensive Care, vol. 8, no. 1, p. 13, 2020.
CrossRef | PubMed
N. Medugu, I. A. Tickler, C. Duru, R. Egah, A. O. James, V. Odili, F. Hanga, E. K. Olateju, B. Jibir, B. E. Ebruke, G. Olanipekun, F. C. Tenover, and S. K. Obaro, "Phenotypic and molecular characterization of Beta-lactam resistant multidrug-resistant Enterobacterales isolated from patients attending six hospitals in Northern Nigeria," Scientific Reports, vol. 13, no. 1, p. 10306, 2023.
CrossRef | PubMed
I. Courti, C. Muja, T. Maho, F. P. Sainct, and P. Guillot, "Degradation of bacterial antibiotic resistance genes during exposure to non-thermal atmospheric pressure plasma," Antibiotics, vol. 11, no. 6, p. 747, 2022.
CrossRef | PubMed
G. D. Wright, "Q&A: Antibiotic resistance: Where does it come from and what can we do about it?" BMC Biology, vol. 8, no. 1, p. 123, 2010.
CrossRef | PubMed
Z. Xu, B. Li, Y. Jiang, J. Huang, L. Su, W. Wu, Q. Pang, Z. Li, J. Zhang, X. Li, J. Wang, F. Cen, L. Peng, J. Liang, F. Wang, C. Liu, C. Shen, Y. Liu, and Y. Yang, "Development of a quadruple qRT-PCR assay for simultaneous identification of hypervirulent and carbapenem-resistant Klebsiella pneumoniae," Microbiology Spectrum, vol. 12, no. 1, p. e0071923, 2024.
CrossRef | PubMed
Q. Luo, L. Xu, Y. Wang, H. Fu, T. Xiao, W. Yu, W. Zhou, K. Zhang, J. Shen, J. Ji, C. Ying, and Y. Xiao, "Clinical relevance, mechanisms, and evolution of polymyxin B heteroresistance carbapenem-resistant Klebsiella pneumoniae: A genomic, retrospective cohort study," Clinical Microbiology and Infection, vol. 30, no. 4, pp. 507–514, 2024.
CrossRef | PubMed
B. Olayiwola, F. O'Neill, C. Frewen, D. F. Kavanagh, R. O'Hara, and L. O'Neill, "Cold plasma deposition of tobramycin as an approach to localized antibiotic delivery to combat biofilm formation," Pathogens, vol. 13, no. 4, p. 326, 2024.
CrossRef | PubMed
M. I. Valdez-Narváez, M. T. Fernández-Felipe, A. Martinez, and D. Rodrigo, "Inactivation of Bacillus cereus spores and vegetative cells in inert matrix and rice grains using low-pressure cold plasma," Foods, vol. 13, no. 14, p. 2223, 2024.
CrossRef | PubMed
A. Helmke, I. Curril, J. Mrotzek, J. Schulz, and W. Viöl, "Non-thermal plasma for decontamination of bacteria trapped in particulate matter filters: Plasma source characteristics and antibacterial potential," Journal of Physics D: Applied Physics, vol. 57, no. 26, p. 265202, 2024.
CrossRef
J. Moszczyńska, K. Roszek, and M. Wiśniewski, "Non-thermal plasma application in medicine-focus on reactive species involvement," International Journal of Molecular Sciences, vol. 24, no. 16, p. 12667, 2023.
CrossRef | PubMed
R. S. Mohammed and M. F. Al-Marjani, "DBD plasma as a practical approach to sterilization of dental instruments," Physica Scripta, vol. 99, no. 4, p. 045601, 2024.
CrossRef
U. Pundjung Juswono, D. J. D. H. Santjojo, R. A. Kasa, and M. Faisal, "Bacterial sterilization using non-thermal plasma method surface dielectric barrier discharge (SDBD): Effect of treatment duration on colony count, DNA, protease enzymes, and cell morphology," Trends in Sciences, vol. 20, no. 7, p. 6760, 2023.
CrossRef
D. Battaggia, Y. Yao, M. N. Nierop Groot, T. Abee, and H. M. den Besten, "Impact of species and strain variability on non-thermal plasma decontamination efficacy," Innovative Food Science & Emerging Technologies, vol. 95, Jul. 2024.
CrossRef
CLSI, “Performance standards for antimicrobial susceptibility testing,” 2023, 33th edition.
Link
N. Petrosillo, F. Taglietti, and G. Granata, "Treatment options for colistin-resistant Klebsiella pneumoniae: Present and future," Journal of Clinical Medicine, vol. 8, no. 7, p. 934, 2019.
CrossRef | PubMed
A. Lührmann, R. Matthes, and A. Kramer, "Impact of cold atmospheric pressure Argon plasma on antibiotic sensitivity of Methicillin-resistant Staphylococcus aureus strains in vitro," GMS Hygiene and Infection Control, vol. 11, Aug. 2016.
CrossRef
L. Guo, R. Xu, Y. Zhao, D. Liu, Z. Liu, X. Wang, H. Chen, and M. G. Kong, "Gas plasma pre-treatment increases antibiotic sensitivity and persister eradication in Methicillin-resistant Staphylococcus aureus," Frontiers in Microbiology, vol. 9, Mar. 2018.
CrossRef | PubMed
T. Gonçalves, A. T. Marques, V. Manageiro, L. Tanoeiro, J. S. Vital, A. Duarte, J. M. Vı́tor, M. Caniça, M. M. Gaspar, and F. F. Vale, "Antimicrobial activity of prophage endolysins against critical Enterobacteriaceae antibiotic-resistant bacteria," International Journal of Pharmaceutics, vol. 651, p. 123758, Feb. 2024.
CrossRef | PubMed
G. Guo, C. Guo, X. Qie, D. He, S. Meng, L. Su, S. Liang, S. Yin, G. Yu, Z. Zhang, X. Hua, and Y. Song, "Correlation analysis between Raman spectral signature and transcriptomic features of carbapenem-resistant Klebsiella pneumoniae," Spectrochimica Acta Part A: Molecular and Biomolecular Spectroscopy, vol. 308, p. 123699, Mar. 2024.
CrossRef | PubMed
J. Julák, E. Vaňková, M. Válková, P. Kašparová, J. Masák, and V. Scholtz, "Combination of non-thermal plasma and subsequent antibiotic treatment for biofilm re-development prevention," Folia Microbiologica, vol. 65, no. 5, pp. 863–869, 2020.
CrossRef | PubMed
Y. Li, L. Wei, J. Lin, Z. Xie, L. Lu, X. Pan, J. Xu, and R. Cai, "Nonthermal plasma air disinfection for the inactivation of airborne microorganisms in an experimental chamber and indoor air," Journal of Applied Microbiology, vol. 135, no. 4, p. lxae078, 2024.
CrossRef | PubMed
E. Vaňková, M. Válková, P. Kašparová, J. Masák, V. Scholtz, J. Khun, and J. Julák, "Prevention of biofilm re-development on Ti-6Al-4V alloy by cometary discharge with a metallic grid," Contributions to Plasma Physics, vol. 59, no. 2, pp. 166–172, 2018.
CrossRef
K. Paul, P. Pandey, U. Rathore, and N. N. Gowda, "Applications of cold plasma technology in the food industry," in Advanced Research Methods in Food Processing Technologies, Apple Academic Press, 2024, pp. 23–37.
CrossRef
J.-W. Lackmann and J. E. Bandow, "Inactivation of microbes and macromolecules by atmospheric-pressure plasma jets," Applied Microbiology and Biotechnology, vol. 98, no. 14, pp. 6205–6213, 2014.
CrossRef | PubMed
H. Lu, S. Patil, K. Keener, P. Cullen, and P. Bourke, "Bacterial inactivation by high-voltage atmospheric cold plasma: Influence of process parameters and effects on cell leakage and DNA," Journal of Applied Microbiology, vol. 116, no. 4, pp. 784–794, 2014.
CrossRef | PubMed
V. Scholtz, E. Vaňková, P. Kašparová, R. Premanath, I. Karunasagar, and J. Julák, "Non-thermal plasma treatment of ESKAPE pathogens: A review," Frontiers in Microbiology, vol. 12, p. 737635, Oct. 2021.
CrossRef | PubMed
A. Privat-Maldonado, D. O'Connell, E. Welch, R. Vann, and M. W. van der Woude, "Spatial dependence of DNA damage in bacteria due to low-temperature plasma application as assessed at the single cell level," Scientific Reports, vol. 6, no. 1, p. 35646, 2016.
CrossRef | PubMed
J. A. Delben, C. E. Zago, N. Tyhovych, S. Duarte, and C. E. Vergani, "Effect of atmospheric-pressure cold plasma on pathogenic oral biofilms and in vitro reconstituted oral epithelium," PLOS ONE, vol. 11, no. 5, p. e0155427, 2016.
CrossRef | PubMed
Downloads
Key Dates
Received
Revised
Accepted
Published
Data Availability Statement
None.
Issue
Section
License
Copyright (c) 2025 Sanaa A. Hamza, Raghad S. Mohammed, Mohammed F. Al Marjani, Mounir M. Bekhit

This work is licensed under a Creative Commons Attribution 4.0 International License.
(Starting May 5, 2024) Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution (CC-BY) 4.0 License that allows others to share the work with an acknowledgement of the work’s authorship and initial publication in this journal.